- Services must be provided to Qualified Medicaid beneficiaries based on individual assessments of need, rather than a one-size-fits-all approach.
- States must assess all available public and private funding streams, including Medicaid, to cover assistance with unmet social needs when developing a strategy for addressing beneficiaries’ SDOH.
- Services provided to address SDOH are limited to those expected to meet the beneficiary’s needs in the most economic and efficient manner possible and are of high quality.
- Each Medicaid service must be sufficient in amount, duration and scope to reasonably achieve its purpose.
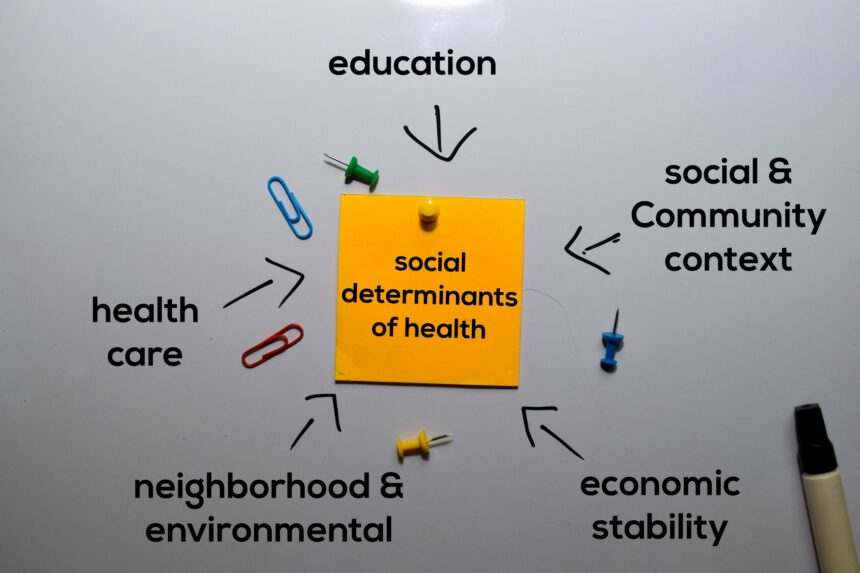
With these overarching principles in mind, the remainder of the announcement focuses on specific services that can be covered under Medicaid and CHIP to address SDOH and mechanisms to deliver these services.
Specific Services Covered, Mechanisms, Eligibility, and Examples
Services ranging from housing and tenancy to home-delivered meals and non-medical transportation are described in the CMS letter to state health officials (SHOs). Officials and their teams are encouraged to dive into the details and uncover all the various ways that CMS is providing official guidance and support here: https://www.medicaid.gov/federal-policy-guidance/downloads/sho21001.pdf. Key federal authorities that can address SDOH and examples of services and supports that can be covered under Medicaid and CHIP are also displayed in table format throughout Appendices A and B.
Through these efforts it becomes abundantly clear that CMS remains committed to partnering with states to address beneficiaries’ SDOH. This is good news for states during trying times and for the foreseeable future as we work together toward the common good: close social gaps in care and address healthcare disparities nationwide.